Abstract
Background: Hepatocytes produce a variety of clotting and fibrinolytic factors. In chronic liver disease (CLD), biosynthesis of these factors is often altered leading to hemostatic aberrations. Recently, the usefulness of PT/INR - one of the five parameters used in the Child-Pugh (CP) scoring system - has been questioned. In this retrospective study, we explored the patterns of plasma alterations relative to CP scores to establish a plasma-based panel that can help evaluate the extent of CLD severity without the use of PT/INR and/or such parameters as the extent of ascites and hepatic encephalopathy.
Methods: Blood was collected via venipuncture (0.129 mol/l sodium citrate) from CLD patients suffering from cirrhosis due to untreated HCV and/or excessive alcohol consumption, that were previously assigned a CP score: CP-A, n=12; CP-B, n=19; CP-C, n=11. Healthy control subjects (n=30) were age and sex matched; all subjects gave informed consent. Within 2 h post-collection, specimens were centrifuged for 15 min at 1500 x g, and then 13000 x g for 2 min to obtain plasma that was immediately frozen at -80°C until used. The following was measured: pro-coagulant phospholipid, fXa, D-dimer, fVIII, sP-selectin, thrombomodulin, protein C, protein S, alternatively spliced Tissue Factor (asTF), free TFPI, TF/TFPI ratio, and TFPI/protein S ratio. Thrombin generation tests (TGT) with and without thrombomodulin were performed. To interrogate the biology of CLD, patient plasma was also analyzed for the levels of microvesicles (MVs) of various origin: endothelium (CD31+/CD41-), monocytes (CD14+), leukocytes (CD11b+), neutrophils (CD16+), platelets (CD41a+, CD41a+/CD62P+, CD62P+), and exosomes (CD63+). Platelet counts and the levels of Annexin V+ MVs were also evaluated. Results were analyzed using GraphPad Prism v.6.03, and the parameters that were significantly different between control and CLD plasma were further evaluated. A system was developed with specified cutoffs for each parameter, derived using clinically normal ranges as well as the data generated in this study, to compile a composite score for CLD severity.
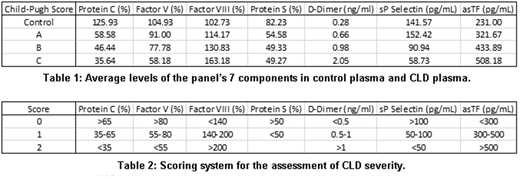
Results: CLD plasma had endogenous thrombin potential comparable to that of control plasma; however, the rate of thrombin generation and peak thrombin generation diminished with increased CLD severity (both p < 0.0001), prolonging the time until peak (p < 0.01) as assessed by TGT. Of the 14 remaining parameters investigated in CLD and control plasma, the levels of fVIII, D-dimer, and asTF increased with CLD severity while protein C, fV, protein S, and sP-selectin levels decreased (Table 1) and in combination, these 7 parameters were able to predict the previously assigned CP scores with high accuracy. Our scoring system assigns a numeric value (0, 1, or 2) for each parameter; a cumulative score of <2 is normal, 2-3 CP-A, 4-7 CP-B, and ≥8 CP-C (Table 2). The system was 97.2% accurate at predicting the CP score: of the 72 plasma samples analyzed, there was only one false positive (a control scored as a CP-A), and one CP-C sample scored as CP-B. Omission of any of the 7 components markedly lowered the system's accuracy. Levels of CD31+/CD41-, CD62+, CD63+, and CD16+ MVs rose with disease severity (p < 0.0001 for all) while CD41a+ MVs decreased (p < 0.0001). Of the panel's 7 components, asTF is relatively novel and so asTF's association with various markers was further examined. There was a positive correlation between asTF and D-dimer (r = 0.305, p = 0.05) and asTF and CD63 (r = 0.346, p = 0.025); asTF negatively correlated with CD14+ MVs (r = -0.348, p = 0.024). There was a strong and highly significant positive correlation between asTF and CD31+/CD41- MVs (r = 0.630, p = 7.81x10-6).
Conclusions: Here we report a novel plasma panel with potential utility in assessing CLD severity in a point-of-care setting. Our scoring system exhibits 97.2% accuracy and does not require clinical assessment beyond plasma analysis. asTF levels positively correlate with those of CD31+/CD41- MVs and both increase with CLD severity; this is in agreement with earlier reports of inflammatory cytokines eliciting asTF secretion from endothelial cells. Larger-scale prospective studies are warranted to validate our findings.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal